What I Learned the Hard Way About Managing Weight with a Chronic Condition
Living with a chronic illness while trying to manage my weight felt like walking uphill in the dark. I thought I was doing everything right—cutting calories, skipping meals, over-exercising—yet I kept hitting walls. My energy crashed, my mood suffered, and the scale barely moved. It wasn’t until I recognized the common missteps that I started seeing real progress. This is what I wish I’d known earlier: small, sustainable changes matter more than extreme fixes. Health isn’t about perfection—it’s about consistency and self-awareness.
The Hidden Challenge: Why Weight Management Feels Harder with Chronic Illness
For many women managing a long-term health condition, the journey to a healthier weight is not just difficult—it’s fundamentally different from the mainstream narrative. Unlike individuals without medical complications, those living with chronic illnesses often face a set of invisible barriers that make traditional weight loss advice ineffective, and sometimes even harmful. Conditions such as type 2 diabetes, hypothyroidism, polycystic ovary syndrome (PCOS), or autoimmune disorders like lupus and rheumatoid arthritis alter the body’s internal environment in ways that affect metabolism, energy levels, and hormonal balance. These changes mean that even with disciplined eating and regular physical activity, progress may be slow or inconsistent.
Fatigue is one of the most underestimated challenges. When your body is constantly fighting inflammation or managing blood sugar fluctuations, the energy required for daily tasks is already stretched thin. Adding intense workouts or strict dietary rules can push the system into further imbalance. Many women report feeling guilty when they can’t maintain the pace promoted by fitness influencers or wellness programs. But the truth is, willpower is not the issue. The body’s altered physiology is. For example, insulin resistance, commonly seen in metabolic and hormonal disorders, makes it harder to burn fat and easier to store it, especially around the abdomen. This isn’t a failure of discipline—it’s a biological response to a medical condition.
Another hidden factor is the emotional toll of chronic illness. Living with constant discomfort, unpredictable symptoms, or the stress of medical appointments can lead to emotional eating or disordered patterns around food. Anxiety and depression, which often accompany long-term health issues, can disrupt sleep and appetite regulation, further complicating weight management. The combination of physical and emotional strain creates a cycle that is hard to break without proper support. Recognizing these challenges is the first step toward developing a kinder, more effective approach—one that works with the body rather than against it.
Pitfall #1: Treating Weight Loss Like a Short-Term Fix
One of the most common mistakes women make is viewing weight management as a temporary project with a clear endpoint—like losing 15 pounds before summer or fitting into an old dress. This mindset leads to extreme measures: skipping meals, following restrictive juice cleanses, or committing to grueling workout routines that are impossible to sustain. While these approaches might yield short-term results, they often backfire, especially for those with chronic conditions. The body interprets severe calorie restriction as a threat, slowing down metabolism to conserve energy. This metabolic adaptation means that even when normal eating resumes, weight can return quickly—sometimes with additional pounds.
For someone already dealing with low energy or hormonal imbalances, this cycle is especially damaging. Pushing through fatigue with intense exercise or prolonged fasting may lead to burnout, increased inflammation, or even flare-ups of underlying conditions. The body needs consistency, not shock tactics. Research shows that gradual, steady changes in eating and movement habits lead to more lasting results than dramatic overhauls. For instance, a study published in the Journal of the American Medical Association found that participants who lost weight slowly—about one to two pounds per week—were more likely to keep it off long-term compared to those who lost weight rapidly.
The shift in thinking must be from “How fast can I lose weight?” to “How can I build a lifestyle that supports my health every day?” This means embracing the idea of health maintenance as a lifelong rhythm. It’s not about reaching a perfect number on the scale and then stopping. It’s about creating daily habits that support energy, mood, and overall well-being, regardless of the pace of weight loss. This approach reduces stress on the body and mind, making it easier to stay consistent even on difficult days. Small choices—like choosing a piece of fruit over a sugary snack, taking a 10-minute walk after dinner, or drinking more water—add up over time and create lasting change without the risk of burnout.
Pitfall #2: Ignoring the Role of Medications and Metabolism
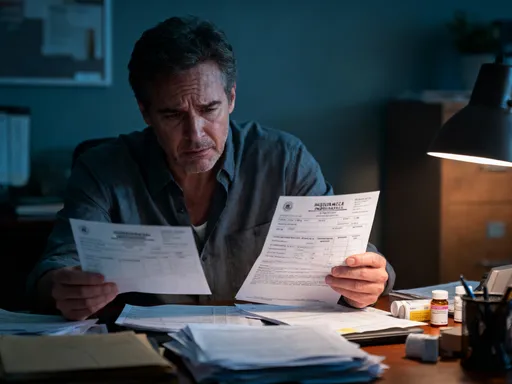
Many women are unaware that the medications they rely on to manage their conditions can significantly impact weight. This is a critical blind spot in most mainstream weight loss advice, which often assumes that everyone’s body responds the same way to diet and exercise. In reality, common treatments for chronic illnesses can alter appetite, fluid retention, fat distribution, and metabolic rate. For example, corticosteroids, often prescribed for autoimmune diseases or severe inflammation, are well-known for causing weight gain, particularly in the face, abdomen, and back of the neck. These changes are not due to overeating—they are a direct side effect of the medication.
Similarly, certain antidepressants and antipsychotic drugs can increase hunger or slow metabolism, making weight management more challenging. Beta-blockers, used for high blood pressure or heart conditions, may reduce resting metabolic rate and make physical activity feel more difficult. Even some diabetes medications, while essential for blood sugar control, can promote fat storage if not balanced with proper nutrition and movement. When women don’t understand these effects, they may blame themselves for lack of progress, not realizing that their medication is working against their weight goals.
The solution is not to stop taking prescribed medications—doing so can be dangerous. Instead, the focus should be on awareness and collaboration. Talking openly with a healthcare provider about weight concerns is essential. Doctors can sometimes adjust dosages, switch to alternative medications with fewer metabolic side effects, or offer strategies to counteract weight gain. Additionally, understanding these factors helps set realistic expectations. If a medication is contributing to fluid retention, for example, daily weight fluctuations are normal and not a sign of failure. The goal is not to eliminate the medication but to work with it, making lifestyle choices that support overall health within the constraints of treatment.
Pitfall #3: Over-Relying on the Scale for Progress
The scale is a misleading tool, especially for women managing chronic illness. It measures only one thing—total body weight—and cannot distinguish between fat, muscle, water, or bone. For someone dealing with inflammation, hormonal shifts, or medication side effects, the number on the scale can fluctuate wildly from day to day, often with no connection to actual fat loss. This creates unnecessary frustration and can lead to discouragement, even when real progress is being made. A woman might be gaining muscle, improving her energy, sleeping better, and fitting into her clothes more comfortably, yet see no change—or even an increase—on the scale.
Body composition is a far more accurate indicator of health. Muscle weighs more than fat but takes up less space, so building lean tissue can lead to a slimmer appearance even if the scale doesn’t move. Additionally, inflammation and fluid retention—common in autoimmune and hormonal conditions—can add several pounds temporarily. These changes are not fat gain, but the scale cannot tell the difference. Relying solely on this single metric ignores the full picture of health and can derail motivation.
A better approach is to use multiple forms of feedback. Tracking non-scale victories provides a more complete and encouraging view of progress. These might include improved stamina, better mood, easier movement, fewer joint pains, or needing to adjust clothing sizes. Weekly check-ins, rather than daily weigh-ins, reduce obsession and allow for natural fluctuations. Using a journal to record how you feel, how your clothes fit, or how many steps you take each day offers valuable insights that the scale cannot. Shifting focus from weight to overall well-being helps maintain motivation and reinforces the idea that health is multidimensional. It’s not about looking a certain way—it’s about feeling stronger, more capable, and more in control of your body.
Pitfall #4: Cutting Out Entire Food Groups Without Guidance
In the age of trendy diets, it’s easy to fall into the trap of eliminating entire food groups—like carbohydrates, fats, or dairy—in the hope of quick weight loss. Popular plans such as keto, paleo, or extreme low-carb diets often promise fast results, but they can be especially risky for women with chronic conditions. These restrictive approaches may lead to short-term weight loss, but they often come at the cost of long-term health. Carbohydrates, for example, are the body’s primary source of energy. Cutting them too drastically can worsen fatigue, impair concentration, and disrupt blood sugar stability—particularly dangerous for those with diabetes or insulin resistance.
Fats are another misunderstood nutrient. Healthy fats from sources like avocados, nuts, seeds, and olive oil play a crucial role in hormone production, brain function, and reducing inflammation. Eliminating them can lead to dry skin, hormonal imbalances, and increased hunger. For women with autoimmune disorders, where inflammation is a key concern, healthy fats are especially important. Similarly, dairy provides calcium and vitamin D, nutrients essential for bone health—critical for women on long-term steroid therapy, which can weaken bones over time.
The real danger of fad diets is that they promote a one-size-fits-all approach, ignoring individual medical needs. What works for one person may harm another. The best path is personalized nutrition—working with a registered dietitian or healthcare provider who understands both weight management and chronic illness. They can help create a balanced, nutrient-dense eating plan that supports energy, stabilizes blood sugar, and reduces inflammation without unnecessary restrictions. Food should be seen as fuel and medicine, not the enemy. A sustainable approach includes a variety of whole grains, lean proteins, vegetables, fruits, and healthy fats, tailored to the body’s unique needs.
Building a Sustainable Routine: Small Shifts That Add Up
Lasting change doesn’t come from dramatic transformations—it comes from small, repeatable habits that fit into real life. For women managing chronic illness, the key is consistency, not intensity. A 10-minute walk after meals, a glass of water with every meal, or adding one extra serving of vegetables to dinner are simple actions that, when repeated daily, create meaningful results over time. These micro-habits are sustainable because they don’t require large amounts of energy or time, making them realistic even on low-energy days.
Mindful eating is another powerful tool. This means paying attention to hunger and fullness cues, eating slowly, and savoring each bite. It helps prevent overeating and improves digestion, both of which support weight management. Hydration is equally important—sometimes thirst is mistaken for hunger, leading to unnecessary snacking. Drinking enough water throughout the day supports metabolism, reduces bloating, and helps the body process nutrients more efficiently.
Sleep hygiene plays a major role as well. Poor sleep disrupts hormones that regulate appetite, increasing cravings for sugar and refined carbs. Aim for 7–8 hours of quality sleep by establishing a calming bedtime routine, limiting screen time before bed, and keeping a consistent sleep schedule. Movement doesn’t have to mean gym sessions—gentle yoga, stretching, or even household chores count as physical activity. The goal is to stay active in ways that feel good, not punishing. On days when energy is low, doing something small is better than doing nothing. Progress isn’t linear, and that’s okay. What matters is showing up for yourself, day after day, with kindness and patience.
The Bigger Picture: Health Maintenance as Self-Respect
At its core, managing weight with a chronic condition is not about appearance—it’s about self-respect and long-term well-being. It’s about feeling strong enough to play with grandchildren, having the energy to enjoy hobbies, and reducing the risk of additional health complications. Health is not a punishment; it’s an act of care. When approached with compassion, small steps become powerful expressions of self-worth. Celebrating progress—whether it’s walking farther, sleeping better, or simply feeling more in control—reinforces positive change and builds confidence.
Patience is essential. The body has been through a lot, and healing takes time. There will be setbacks, flare-ups, and days when motivation is low. That’s normal. What matters is the overall direction. Seeking support from healthcare professionals, dietitians, or support groups can provide guidance and encouragement. No one should have to navigate this journey alone. Every choice that supports health—no matter how small—is a victory. This is not about perfection. It’s about showing up, being consistent, and honoring the body’s needs with kindness and respect. In the end, true health is not measured by a number, but by how you feel every day.