How I Nailed My Recovery: Real Talk on Meds and Knowing Your Body
When I started my rehab journey, I had no clue how much my relationship with medication would change. It wasn’t just about taking pills—it was about understanding my body, tracking progress, and staying honest with myself. Through trial and small wins, I learned that effective treatment isn’t one-size-fits-all. This is my take on making medication work *with* you, not just *for* you—plus how health checks became my secret weapon.
The Moment Everything Changed
The call came on a Tuesday afternoon. The doctor’s voice was calm, but the words landed like stones: a diagnosis that changed everything. At first, I didn’t know whether to cry, to call a friend, or to just sit in silence. The condition wasn’t life-threatening, but it was life-altering. Simple things—walking up the stairs, lifting a grocery bag, even sleeping through the night—became uncertain. I remember staring at the prescription slip, the name of the medication unfamiliar, the dosage instructions a blur. It felt like signing a contract with no fine print.
There was fear, yes, but also confusion. What did this pill actually do? How long before I’d feel better? Could I still drink coffee? Could I keep working? No one had given me a clear roadmap. I followed the instructions blindly, swallowing the first dose with a glass of water and a quiet prayer. For weeks, I waited for a miracle. But healing doesn’t arrive in a bottle. I soon realized that medication was only one thread in a much larger tapestry. The early days were marked by trial and error, missed side effects, and moments of doubt. I wasn’t just healing my body—I was relearning how to listen to it.
What I didn’t know then was that recovery isn’t passive. It doesn’t happen simply because you take a pill at the same time every day. True progress required awareness, patience, and a willingness to ask hard questions. My turning point wasn’t a sudden improvement in symptoms—it was the moment I stopped seeing myself as a patient and started seeing myself as a participant. That shift didn’t come from a doctor’s note. It came from paying attention.
Why “Just Take the Pill” Isn’t Enough
Medication is often presented as the solution, the endpoint of a medical journey. But for many people managing chronic conditions or recovering from injury, it’s only the beginning. The phrase “just take the pill” oversimplifies a complex reality. Pills don’t operate in a vacuum. They interact with sleep, diet, stress levels, and even the time of day they’re taken. Yet, too often, patients are sent home with little more than a prescription and a vague instruction to “follow up in six weeks.”
Understanding dosage timing, for example, is more important than many realize. Some medications are more effective when taken with food, while others must be taken on an empty stomach. Missing that detail can reduce effectiveness by up to 50%, according to clinical pharmacology studies. Side effects are another under-discussed factor. Fatigue, nausea, or mood shifts aren’t just inconveniences—they can derail daily life if not anticipated and managed. Without clear guidance, many people stop taking their medication not because it doesn’t work, but because the side effects feel worse than the condition itself.
The deeper issue is a lack of treatment context. Why is this medication being prescribed? What does success look like? How long should it take to notice changes? When patients don’t understand the goals, they can’t track progress meaningfully. This leads to frustration, disengagement, and sometimes, premature discontinuation. Medication works best when it’s part of a broader strategy—one that includes self-monitoring, lifestyle adjustments, and open communication with healthcare providers. Taking a pill is an action. Healing is a process.
My First Real Health Check-Up (And What I Learned)
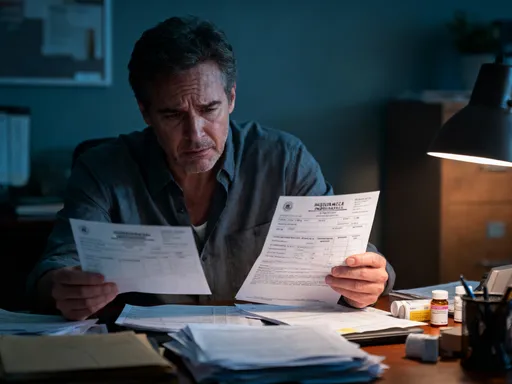
My first comprehensive health assessment came three months into treatment. Up until then, I’d only had brief follow-ups focused on whether my symptoms had improved. But this visit was different. It lasted over an hour and included blood work, joint mobility tests, a sleep quality questionnaire, and even a mood tracking review. I was asked about energy levels, digestion, stress, and daily function—not just pain.
The results were eye-opening. My blood markers showed mild inflammation, which explained the lingering stiffness. My vitamin D was low, a common issue that can worsen musculoskeletal recovery. The mobility test revealed imbalances I hadn’t noticed—my right hip was significantly tighter than the left, likely due to unconscious compensation. And the mood tracker, which I’d filled out weekly, showed a clear pattern: on days when I slept poorly, my pain perception spiked, even if my activity level was the same.
For the first time, I saw my condition not as a single problem, but as a network of interconnected factors. The medication was helping, but it wasn’t addressing the full picture. The doctor didn’t suggest stopping the pills—in fact, they reaffirmed their importance. But they also recommended adding targeted physical therapy, adjusting my supplement intake, and prioritizing sleep hygiene. This wasn’t a rejection of medication; it was an expansion of care. I left that appointment not with a new drug, but with a new mindset: healing requires data, not just drugs.
3 Game-Changing Habits That Made My Meds Work Better
Once I understood that medication was just one piece of the puzzle, I began looking for ways to support its effectiveness. Three habits, in particular, made a measurable difference—not only in how I felt day to day, but in how consistently my treatment worked.
The first was **consistent sleep timing**. I used to go to bed at different times, especially on weekends. But research shows that irregular sleep can disrupt hormone regulation, including cortisol and melatonin, both of which influence inflammation and pain perception. By setting a fixed bedtime and wake time—even on Saturdays—I noticed improved energy, fewer morning aches, and better medication response. Sleep isn’t just rest; it’s repair time for the body.
The second habit was **food-med interaction awareness**. I learned that one of my medications was less effective when taken with dairy, as calcium can interfere with absorption. Another worked better when paired with healthy fats, which aid in nutrient uptake. I started reading labels, spacing out meals and meds when needed, and keeping a simple log of what I ate and when I took my pills. This small change led to fewer side effects and more predictable results.
The third and most powerful habit was **symptom journaling**. Every evening, I spent five minutes writing down my pain level, mood, energy, and any side effects. At first, it felt tedious, but within weeks, patterns emerged. I saw that stress at work often preceded flare-ups. I noticed that days with gentle movement—like walking or stretching—were followed by better sleep and improved medication response. This journal became my personal feedback loop, helping me adjust my routine before problems escalated.
When the Plan Failed—And What I Did Next
About eight months into recovery, I hit a wall. The medication that had been working steadily suddenly seemed less effective. Pain crept back, fatigue returned, and my mood dipped. I felt defeated. My first instinct was to blame myself—had I slipped up on my habits? Was I not trying hard enough? For a few days, I considered stopping the medication altogether. But instead, I scheduled a follow-up appointment.
The doctor explained that this kind of plateau is common. The body can adapt to certain medications over time, reducing their impact. In some cases, underlying factors—like stress, hormonal shifts, or nutritional gaps—can change, altering how treatment works. The solution wasn’t to quit, but to reassess. We reviewed my journal, ran another round of blood work, and discussed recent life changes. It turned out I’d been under more stress than I realized, and my vitamin B12 was low, which can contribute to fatigue and nerve sensitivity.
We adjusted my supplement plan, added a short course of physical therapy to address the stiffness, and fine-tuned the timing of my medication. I also began incorporating mindfulness exercises to manage stress. Within weeks, the progress returned. This experience taught me that setbacks aren’t failures—they’re signals. They don’t mean you’re doing something wrong; they mean it’s time to gather new information and adapt. Healing isn’t linear, and flexibility is part of the process.
How I Track Progress Without Obsessing Over It
Tracking can be powerful, but it can also become overwhelming. Early on, I made the mistake of measuring everything: steps, heart rate, sleep cycles, pain levels, even water intake. I was drowning in data. I’d wake up and immediately check my numbers, feeling anxious if they weren’t “perfect.” That kind of hyper-vigilance isn’t sustainable—and it’s not helpful.
I’ve since simplified my approach. Now, I do a brief weekly check-in. Every Sunday evening, I spend ten minutes reviewing three key areas: energy, function, and mood. I rate each on a scale of 1 to 10 and jot down a few notes. Did I complete my daily walk? Could I carry groceries without discomfort? Did I feel calm most of the week? I use a small notebook—no apps, no notifications. This keeps it low-pressure and personal.
The goal isn’t perfection, but pattern recognition. If I notice two or three weeks of declining energy, I don’t panic. I look for possible causes: poor sleep, increased stress, missed doses. Then I make a small adjustment. Maybe I go to bed 30 minutes earlier. Maybe I reschedule a busy day. Tracking isn’t about control—it’s about awareness. And when done gently, it builds confidence, not anxiety. I’ve learned to celebrate small wins: a good night’s sleep, a pain-free morning, a moment of ease in movement. Those are the real markers of progress.
Putting It All Together: My Daily Reality Now
Today, my routine is structured but flexible. I take my medication at the same time each morning, always with a light meal that supports absorption. I’ve kept my sleep schedule consistent, and I still journal weekly. But the biggest change is internal: I trust myself more. I know the difference between a temporary setback and a real warning sign. I can adjust my day based on how I feel, without guilt or fear.
My doctor visits are less frequent now—every four months instead of every six weeks. Not because my condition is gone, but because my management is more effective. I come to appointments with data, questions, and observations. I’m not just receiving care; I’m co-creating it. That partnership has made all the difference.
Recovery hasn’t meant returning to who I was before. It’s meant becoming someone new—someone more attentive, more resilient, more in tune with their body. Medication still plays a role, but it’s no longer the center of my world. It’s one tool among many: sleep, movement, nutrition, mindfulness, and self-awareness all have their place. The journey isn’t over. Some days are still hard. But now, I have the tools to meet them.
Success isn’t the absence of symptoms. It’s the presence of confidence. It’s knowing you can adapt, respond, and keep moving forward. That’s the kind of recovery that lasts.
Medication is a valuable tool, but it is not a standalone solution. True healing happens when treatment is combined with self-knowledge, consistent habits, and honest reflection. Every body responds differently, and what works today may need adjustment tomorrow. The key is to stay engaged—not just with your prescription, but with your entire well-being. By embracing both medical guidance and personal insight, you take ownership of your health in a meaningful way. Progress may be slow, but it is steady when built on awareness and care. The journey is ongoing, but each small step strengthens your resilience for the long term.