How I Tamed My Lipids and Reclaimed My Energy – A Real Recovery Journey
Ever feel like your body’s running on low battery, no matter how much you rest? That was me—until I discovered my lipid levels were silently working against me. It wasn’t just about cholesterol; it was about how I felt every single day. This isn’t a medical fix, but my honest journey of adjusting habits, seeing real shifts, and slowly rebuilding my vitality. If you're tired of feeling off and want to understand what you can do, this is for you. Always consult your doctor—but small changes? They can add up in ways I never expected.
The Wake-Up Call: When Normal Feels Anything But
For years, I thought I was doing fine. I ate what I considered balanced meals, avoided smoking, and walked occasionally. I wasn’t overweight, and I didn’t have chest pain or any alarming symptoms. Yet, I was constantly tired—like I was dragging myself through the day. Mornings felt heavy. Afternoons were worse. I’d reach for coffee not because I enjoyed it, but because I needed it. My concentration slipped during simple tasks, and I often felt irritable without understanding why.
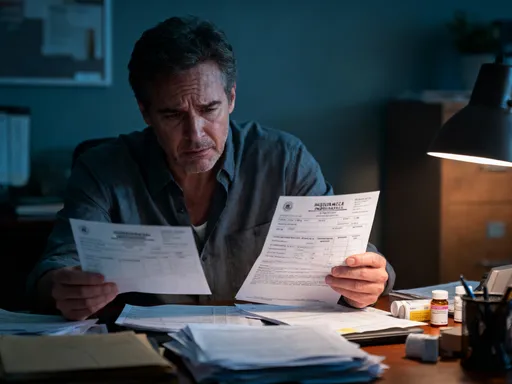
The turning point came during a routine check-up. My doctor reviewed my blood work and paused. My lipid panel showed elevated LDL cholesterol and borderline high triglycerides. To be clear, I wasn’t in crisis, but the numbers were outside the optimal range. What struck me most was the doctor’s calm explanation: “You may not feel sick, but over time, this can affect your heart health and how your body functions every day.” That phrase—how your body functions—stuck with me. I wasn’t just tired; my internal systems were under quiet strain.
What surprised me was how invisible the issue felt. High lipids don’t announce themselves with pain or fever. They don’t show up in mirrors. Instead, they whisper through fatigue, brain fog, and a general sense of being off. I began to realize that “normal” lab results don’t always mean optimal health. My body wasn’t failing—it was sending signals, and I’d been too busy to listen. That moment wasn’t about fear; it was about awareness. And from that awareness, a quiet determination grew: I wanted to feel better, not just avoid disease.
I didn’t leave the office with a prescription that day. Instead, I left with a choice—to make changes now or wait for something more serious later. I chose now. Not because I was desperate, but because I deserved to feel vibrant, clear-headed, and energized. This wasn’t about fixing a broken body; it was about honoring the one I had by giving it what it truly needed.
What Lipids Really Do in Your Body (And Why Balance Matters)
To understand what was happening inside me, I had to learn what lipids actually do. At first, I thought of cholesterol as something to eliminate, like a toxin. But the truth is far more nuanced. Lipids—primarily cholesterol and triglycerides—are essential components your body uses every day. They help build cell membranes, produce hormones like estrogen and testosterone, and support brain function. Without them, your body couldn’t function at all.
The key isn’t eliminating lipids but managing their balance. Think of your bloodstream like a delivery system. Low-density lipoprotein, or LDL, carries cholesterol from the liver to the cells. When there’s too much, it can leave behind deposits in the artery walls—like delivery trucks spilling cargo along the road. Over time, this buildup can narrow blood vessels and reduce circulation. High-density lipoprotein, or HDL, acts like a cleanup crew, picking up excess cholesterol and bringing it back to the liver for disposal. So while LDL is often labeled “bad,” and HDL “good,” it’s not that simple. It’s about proportion, quality, and how your body processes them.
Triglycerides are another type of fat that stores excess energy from your diet. When you eat more calories than your body needs, it converts those calories into triglycerides, which circulate in the blood and are stored in fat cells. Chronically high levels—often linked to diets high in refined sugars and carbohydrates—can contribute to inflammation and metabolic stress. The problem isn’t the fat itself; it’s the overload.
What many people don’t realize is how this internal balance affects daily life. Poor lipid metabolism can reduce blood flow to the brain, leading to mental fatigue and difficulty focusing. It can make muscles feel heavier because oxygen and nutrients aren’t moving efficiently. Over time, this imbalance increases the risk of cardiovascular issues, but long before that, it affects how you feel waking up, working, and moving through your day. The body is interconnected—what happens in the bloodstream doesn’t stay there. It echoes in your energy, mood, and clarity.
Understanding this shifted my mindset. I wasn’t fighting a villain; I was supporting a system. My goal wasn’t to erase cholesterol but to help my body manage it better. This wasn’t about perfection—it was about creating conditions where balance could return naturally.
The Food Shifts That Actually Made a Difference
When I decided to make changes, food was the first place I looked. I didn’t want to follow a strict diet or eliminate entire food groups. Instead, I focused on gradual shifts—small choices that could become sustainable habits. The biggest change was moving away from processed foods and toward whole, nutrient-dense options. I didn’t do it perfectly, but consistency mattered more than perfection.
One of the first swaps was replacing butter with olive oil. I started using extra virgin olive oil for cooking and in salad dressings. It’s rich in monounsaturated fats, which research shows can support healthy cholesterol levels when used in place of saturated fats. I also began adding more fiber to my meals—starting with oats for breakfast. Oats contain beta-glucan, a type of soluble fiber that helps reduce LDL cholesterol by binding to it in the digestive tract and carrying it out of the body.
I increased my intake of legumes—beans, lentils, chickpeas—adding them to soups, salads, and grain bowls. These are excellent sources of plant-based protein and fiber, both of which help regulate blood sugar and support healthy lipid metabolism. I also started choosing plain Greek yogurt instead of flavored versions, then adding fresh fruit for sweetness. This simple change cut out a lot of added sugar, which I later learned plays a major role in raising triglycerides.
Nuts became my go-to snack. A small handful of almonds or walnuts provided healthy fats, protein, and a satisfying crunch. I avoided salted or sugared varieties and kept portions moderate—about a quarter cup per serving. Avocados also became a staple, whether sliced on toast or blended into smoothies. These foods didn’t feel like restrictions; they felt like upgrades.
I didn’t ban treats. I still enjoy dark chocolate, a slice of cake at family gatherings, or an occasional glass of wine. The difference is intentionality. I no longer reach for snacks out of habit or boredom. I plan meals ahead when possible, though some weeks are better than others. Meal prepping on Sundays helps, but I’ve learned to forgive myself when life gets busy. Progress isn’t linear, and that’s okay.
Over time, these changes began to show. I had more stable energy throughout the day. I wasn’t crashing after lunch. And when I had my blood work repeated six months later, my LDL had dropped, and my HDL had improved slightly. My doctor noted the positive trend and encouraged me to keep going. It wasn’t magic—it was consistency.
Moving More Without Burning Out
Exercise used to feel like another chore—something I should do but never enjoyed. I tried intense workouts before, but they left me sore and unmotivated. This time, I redefined movement. Instead of aiming for an hour at the gym, I focused on fitting in small bursts of activity throughout the day. The goal wasn’t to burn calories; it was to support my body’s natural ability to process fats and improve circulation.
I started walking—simple, accessible, and effective. I began with 10-minute walks after meals, especially dinner. Research shows that light activity after eating helps the body manage blood sugar and triglyceride levels more efficiently. Over time, those 10 minutes became 20, then 30. I didn’t track steps obsessively, but I noticed I was walking more naturally—parking farther away, taking the stairs, walking while on phone calls.
I also added gentle stretching at home. Every morning, I spent five to ten minutes doing basic movements—reaching for the sky, touching my toes, rolling my shoulders. It helped me wake up and improved my posture. On weekends, I tried short yoga videos online. Nothing advanced—just slow, mindful movements that helped me feel more connected to my body.
There were days I skipped. Weeks when the weather was bad or my schedule was tight. I used to feel guilty, but I’ve learned that rest is part of the process. The key is restarting without judgment. I remind myself that one missed walk doesn’t erase progress. What matters is the overall pattern.
Surprisingly, movement began to support other areas of my health. I slept better. My mood improved. I felt less stiff and more capable. It wasn’t about pushing harder—it was about showing up consistently, in ways that felt good. Movement became less of a task and more of a gift to myself.
Sleep, Stress, and the Hidden Lipid Triggers
As I made changes to food and movement, I began to notice something unexpected: my stress levels and sleep quality were just as important as diet and exercise. I had always thought of heart health as being about cholesterol and exercise, but I didn’t realize how deeply stress and poor sleep could disrupt metabolic balance.
Chronic stress triggers the release of cortisol, a hormone that, in excess, can increase fat storage and raise triglyceride levels. When I was overwhelmed—juggling work, family, and household tasks—my body stayed in a low-grade state of alert. I didn’t feel anxious, but I was always “on.” That constant activation affects how the body processes fats and sugars. Even with good food choices, stress can undermine progress.
Sleep played a similar role. When I didn’t get enough rest, I craved more carbohydrates and felt sluggish the next day. Poor sleep disrupts hormones that regulate hunger and metabolism, making it harder to maintain healthy lipid levels. I realized I was getting only six hours a night—just enough to function, not enough to thrive.
To address this, I created a simple bedtime routine. I turned off screens an hour before bed, replaced them with reading or light stretching. I kept my bedroom cool and dark. I stopped drinking coffee after noon. These changes didn’t fix everything overnight, but over weeks, I began falling asleep faster and waking up feeling more refreshed.
I also started practicing mindful breathing. When I felt overwhelmed, I’d pause and take five slow, deep breaths. It wasn’t a cure-all, but it helped me reset. I began to see emotional well-being as part of physical recovery. Calming the mind didn’t just reduce stress—it helped regulate the body from the inside out.
Tracking Progress Beyond the Scale
One of the most freeing decisions I made was to stop obsessing over the scale. Weight can be a factor in lipid health, but it’s not the only measure of progress. I shifted my focus to how I felt day to day. I started noticing small victories: climbing stairs without getting winded, concentrating during a long meeting, feeling alert in the afternoon instead of reaching for a snack.
I kept a simple journal—not to track calories or exercise, but to note energy levels, mood, and sleep quality. Over time, patterns emerged. On days I walked, ate well, and slept enough, I felt sharper and more balanced. On days I skipped movement or stayed up late, I felt heavier, mentally and physically.
When I had my blood work repeated, I looked at the trends, not just the numbers. My doctor emphasized that changes take time. It took three months to see a modest improvement, and another three for more noticeable shifts. There were no dramatic drops, but the direction was positive. More importantly, I felt different. I wasn’t just managing lipids—I was reclaiming my vitality.
The scale didn’t change much, but my clothes fit better. My skin looked clearer. I had more patience with my family. These weren’t just physical changes—they were signs of deeper healing. Progress wasn’t about perfection; it was about presence. I was more in tune with my body, and that awareness became its own reward.
Building a Lifestyle That Stays—Without Going Extreme
Looking back, the most important lesson wasn’t about food or exercise—it was about mindset. I used to believe that health required drastic changes: strict diets, punishing workouts, complete deprivation. But what actually worked was the opposite: small, sustainable choices that fit into my real life.
I didn’t transform overnight. I didn’t eliminate all sweets or become a fitness enthusiast. Instead, I integrated habits gradually—like adding oats to breakfast, walking after dinner, or turning off screens before bed. These weren’t rules; they became rhythms. And because they felt manageable, I stuck with them.
Flexibility has been key. I allow myself treats, rest days, and imperfect moments. Life isn’t predictable, and health shouldn’t depend on perfection. What matters is the overall pattern—the choices I make most of the time.
This journey wasn’t about fixing a problem. It was about building a life where my body could thrive. I still see my doctor regularly and get blood work done. I stay informed, but I don’t obsess. I’ve learned to trust the process and listen to my body.
If you’re feeling tired, foggy, or just not like yourself, know this: you’re not alone. Small changes can lead to real shifts. You don’t have to do everything at once. Start with one thing—swap one snack, take one walk, go to bed 15 minutes earlier. These choices add up. They did for me. And with time, patience, and self-compassion, you can reclaim your energy too. Always consult your healthcare provider, but remember: you have more power than you think. Your body is designed to heal. Sometimes, it just needs the right support.